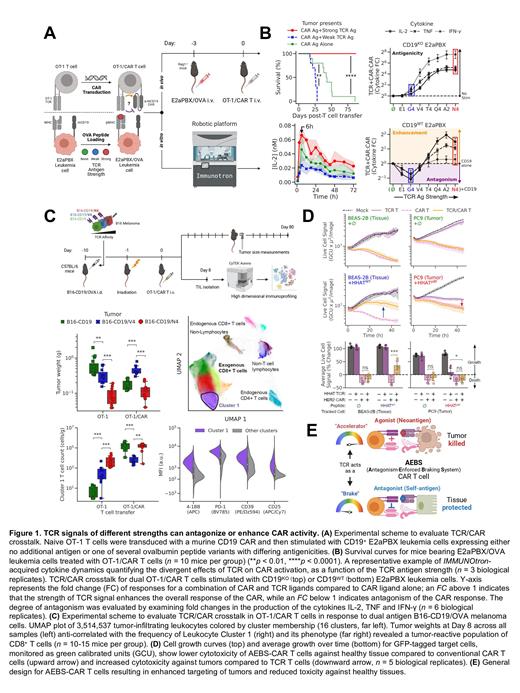
Chimeric Antigen Receptor (CAR) T cell immunotherapy represents a conceptual breakthrough in the treatment of hematological malignancies. However, the rarity of cell surface protein targets specific to cancerous but not vital tissue has hindered its broad application to solid tumor treatment. While new logic-gated CAR designs have shown reduced toxicity against healthy tissues, the generalizability of such approaches across tumors remains unclear. Here, we harness a universal characteristic of endogenous T cell receptors (TCRs), their ability to discriminate between self and non-self ligands through inhibition of response against self (weak) antigens, to develop a broadly applicable method of enhancing immunotherapeutic precision. We hypothesized that this discriminatory mechanism, known as antagonism, would apply across receptors, allowing for a transfer of specificityfrom TCRs onto CARs. We therefore systematically mapped out the responses of CAR T cells to joint TCR and CAR stimulations. We transduced ovalbumin-specific TCR T cells with mouse CD19 CAR to produce T cells expressing both TCR and CAR and evaluated the response of TCR/CAR T cells using in vivo and in vitro leukemia models ( Figure 1A). We discovered that strong TCR antigen enhanced CAR T killing of CD19 + leukemia, while weak TCR antigen antagonized CAR T responses as assessed in vivo cytotoxicity and in vitro multiplexed dynamic profiling ( Figure 1B). We developed a mathematical model based on cross-receptor inhibitory coupling that accurately predicted the extent of TCR/CAR antagonism across a wide range of immunological settings. This model was validated in a CD19 + B16 mouse melanoma model showing that TCR/CAR antagonism decreased the infiltration of a tumor-reactive T cell cluster (cluster 1), while TCR/CAR agonism enhanced infiltration of this cluster1 ( Figure 1C). We then applied our quantitative knowledge of TCR/CAR crosstalk to design an Antagonism-Enforced Braking System (AEBS) for CAR T cell therapy. This was assessed in a model system using a CAR targeting the tyrosine-protein kinase erbB-2 (HER2), expressed on a subset of patients with both B-ALL and AML together with a hedgehog acyltransferase (HHAT) specific TCR, which responds strongly to mutated peptides presented on tumor cells and weakly to wild-type peptides presented on healthy tissue. Consistent with our discovery of the TCR/CAR antagonism, TCR signals against healthy cells expressing wild-type HHAT peptide antigen antagonized HER2 CAR T cell responses, minimizing on-target/off-tumor cytotoxicity against healthy cells. Notably though, AEBS-CAR T cells exhibited high anti-tumor cytotoxicity against tumor cells expressing HER2 and mutated HHAT peptides ( Figure 1D). AEBS CAR T cells sharpen the discriminatory power of synthetic anti-tumor lymphocytes, laying the groundwork for future studies to engineer complex logic into cells with minimal numbers of receptors ( Figure 1E). Our work highlights a novel mechanism by which TCRs can enforce CAR T cell specificity, with practical implications for the rational design of future anti-leukemia immunotherapies.
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal